Coronary artery disease (CAD) is a leading cause of death worldwide. This condition arises when the arteries supplying blood to the heart muscle—the coronary arteries—become narrowed or blocked.
The culprit behind this narrowing is atherosclerosis, a process where fatty deposits, known as plaques, accumulate within the artery walls. These plaques can progressively restrict blood flow, leading to chest pain (angina), shortness of breath, and in severe cases, heart attacks.
While lifestyle changes and medications can help manage CAD, angioplasty offers a powerful tool for physically opening blocked arteries and restoring vital blood flow to the heart.
What is Angioplasty?
Angioplasty, also known as percutaneous transluminal coronary angioplasty (PTCA), is a minimally invasive procedure designed to open narrowed or blocked coronary arteries. The term "percutaneous" signifies that the procedure is performed through the skin, "transluminal" indicates that access is gained through the blood vessel, and "angioplasty" refers to the repair of the vessel.
Unlike open heart surgery, angioplasty doesn't require a large chest incision. Instead, it utilizes a small puncture in an artery, usually in the groin or wrist, to access the coronary arteries.
The Angioplasty Procedure
The angioplasty procedure typically involves the following steps:
- Accessing the Artery: A small incision is made in the groin or wrist to access a large artery, typically the femoral or radial artery.
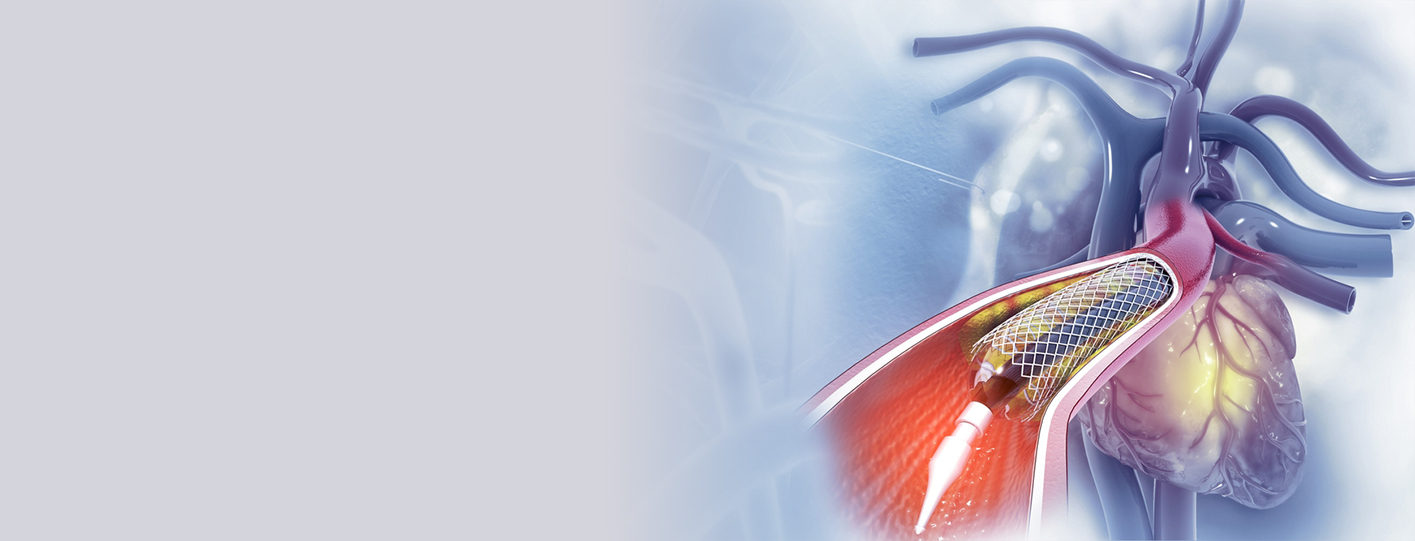
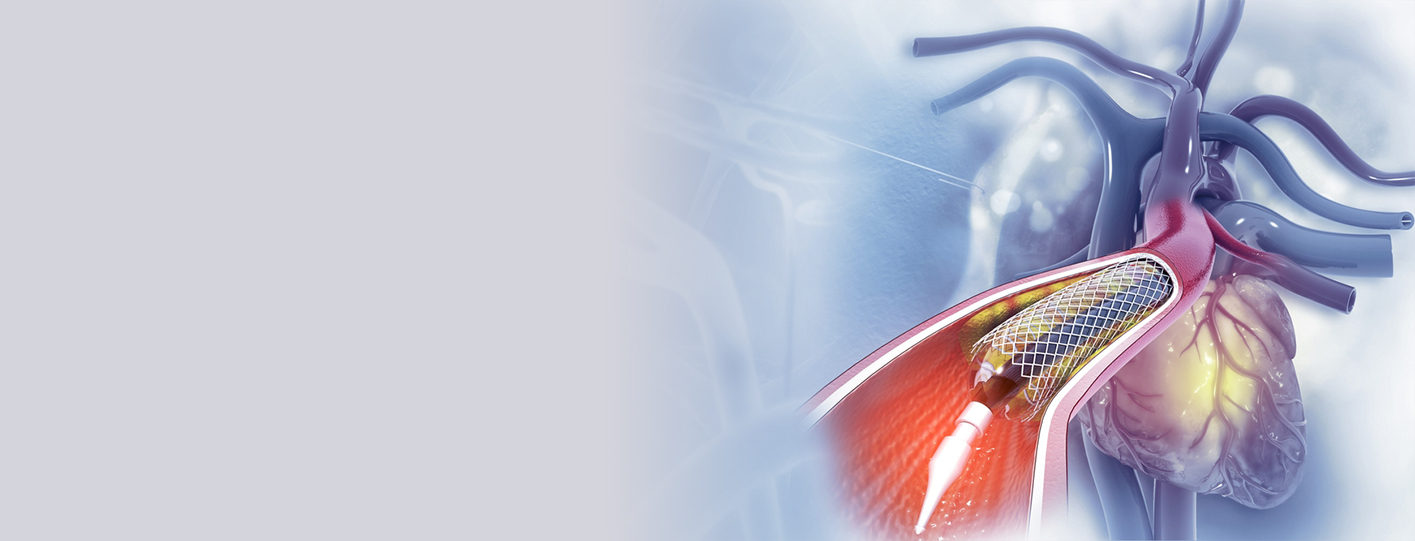
- Catheter Insertion: A thin, flexible tube called a catheter is inserted through the incision and carefully guided towards the coronary arteries. Throughout the procedure, real-time X-ray imaging (fluoroscopy) is used to visualize the catheter's progress and ensure accurate placement.
- Locating the Blockage: Once the catheter reaches the coronary arteries, a contrast dye is injected. This dye highlights the arteries on the X-ray images, allowing the interventional cardiologist to pinpoint the exact location and severity of the blockage. This process is called coronary angiography.
- Balloon Inflation: A second, specialized catheter with a small, inflatable balloon at its tip is then advanced over the guide wire to the site of the blockage. The balloon is inflated, compressing the plaque against the artery walls and widening the vessel to restore blood flow.
- Stent Placement (Most Cases): In most angioplasty procedures, a stent—a small, expandable, mesh-like tube—is deployed at the site of the blockage. The stent acts as a scaffold, providing support to the artery walls and helping to prevent the artery from narrowing again (restenosis). The stent is typically placed after the balloon is deflated, remaining permanently in place.
What is Complex Coronary Angioplasty?
While standard angioplasty is highly effective for many patients with CAD, certain blockages present unique challenges. These complex lesions require specialized techniques and expertise to achieve successful outcomes. Some examples of complex coronary artery blockages include:
- Chronic Total Occlusions (CTOs): These are complete blockages of a coronary artery that have been present for three months or longer. CTOs are often more difficult to treat than partial blockages because the artery may be completely closed off, making it challenging to pass a guidewire through the blockage.
- Bifurcation Lesions: These are blockages that occur at the branching point (bifurcation) of two arteries. Treating bifurcation lesions requires careful planning and specialized techniques to ensure that blood flow is restored to both branches.
- Severely Calcified Arteries: In some patients, the plaques within the coronary arteries become heavily calcified (hardened by calcium deposits). Calcified plaques can be difficult to compress with a balloon, making it challenging to place a stent effectively.
- Left Main Coronary Artery Disease: Blockages in the left main coronary artery, which supplies a significant portion of blood to the heart, are considered high-risk and often require specialized treatment strategies.
- Prior Stent Restenosis: Sometimes, a previously placed stent can become narrowed again (restenosis). Treating in-stent restenosis can be complex, particularly if the restenosis is severe or involves multiple areas within the stent.
What are Specialized Techniques in Complex Coronary Angioplasty
To overcome the challenges posed by complex coronary lesions, interventional cardiologists employ a range of specialized techniques, including:
- Rotational Atherectomy: This technique is used to treat severely calcified plaques. A high-speed rotating device, often referred to as a "burr," is used to grind away the hard calcium deposits, creating a channel through which a balloon and stent can be passed.
- Laser Atherectomy: In this technique, a laser catheter is used to vaporize or break down the plaque, making it easier to dilate the artery with a balloon and place a stent.
- Chronic Total Occlusion (CTO) Techniques: Treating CTOs requires specialized guidewires, catheters, and techniques. Interventional cardiologists often use a variety of strategies to cross the complete blockage, including using specialized guidewires with different tip shapes and stiffnesses, as well as techniques like retrograde crossing (approaching the blockage from a different artery).
- Intravascular Imaging (IVUS/OCT): Intravascular ultrasound (IVUS) and optical coherence tomography (OCT) are imaging techniques that provide detailed images of the inside of the coronary arteries. These techniques can be particularly useful in complex cases, helping the interventional cardiologist to assess the severity of the blockage, guide stent placement, and confirm optimal stent expansion.
Benefits of Complex Coronary Angioplasty
The benefits of complex coronary angioplasty are substantial for patients with challenging coronary artery blockages:
- Symptom Relief: Opening blocked arteries improves blood flow to the heart muscle, alleviating symptoms such as chest pain (angina) and shortness of breath.
- Improved Quality of Life: By reducing symptoms and improving heart function, complex angioplasty can significantly enhance a patient's quality of life, allowing them to return to their normal activities.
- Reduced Need for More Invasive Procedures: In many cases, complex angioplasty can avoid the need for more invasive procedures, such as open-heart surgery (coronary artery bypass grafting or CABG).
Are There Any Risks Associated with Complex Coronary Angioplasty?
While complex coronary angioplasty is generally safe and effective, it's essential to be aware of the potential risks and complications:
- Restenosis: The risk of restenosis (re-narrowing of the artery) is present after any angioplasty procedure, including complex angioplasty. However, the use of drug-eluting stents (stents coated with medication that helps to prevent restenosis) has significantly reduced this risk.
- Stent Thrombosis: Blood clots can form within the stent, a potentially serious complication known as stent thrombosis. Antiplatelet medications are prescribed after angioplasty to help prevent stent thrombosis.
- Bleeding: Bleeding can occur at the catheter insertion site.
- Other Risks: Other potential risks include heart attack, stroke, and damage to the artery.
Recovery and Aftercare
After complex coronary angioplasty, patients are typically monitored in the hospital for a period of time. Most patients can return to their normal activities within a week or two. It's crucial to follow the healthcare provider's instructions regarding medications, lifestyle changes, and follow-up appointments.